What is Blepharospasm?
Also known as Benign Essential Blepharospasm, it is a condition that causes involuntary squeezing of the muscles in the eyelids, including the frown muscles. In some patients, other facial muscles may also be involved. Patients with blepharospasm generally have dry eyes and the spasms are exacerbated by bright lights.
Blepharospasm.
Patel B.C.K., Anderson R.L.
Ophthalmic Practice 1993; 11: 293-312.
Blepharospasm and related facial movement disorders.
Patel B.C.K., Anderson R.L.
Current Opinion in Ophthalmology 1995;6:86-99.
Patel B.C.K., Anderson R.L.
Ophthalmic Practice 1993; 11: 293-312.
Blepharospasm and related facial movement disorders.
Patel B.C.K., Anderson R.L.
Current Opinion in Ophthalmology 1995;6:86-99.
"Well, the last time I had a picture taken I could hardly see my eyes because of the weight of heavy eyelid. Then I paid attention to how I was actually using my eyes and I really noticed when I was looking at anything especially the computer I was straining my forehead to see better. Since I have had it done I no longer have to lift the forehead and tilt my head to see. It is amazing! I love..." D. Rock 63 Yrs Old with Fat Droopy Eyes - Salt Lake City, UT
|
|
How does blepharospasm present?The earliest sign of blepharospasm is a simple increase in the blink rate with only intermittent eyelid spasms: this is often missed and patient may be diagnosed with a neuropsychiatric disorder like depression or anxiety. Over time this increases to more uncontrolled spasms. If untreated, the spasms are severe enough to make people functionally blind with severe overaction of the facial muscles and may also lead to depression.
|
What is apraxia of eyelid opening?A certain number of patients with blepharospasm will have difficulty opening their eyelids and they find themselves struggling to open the eyelids by raising their brows. In some of these patients, the degree of squeezing is not severe.
A certain number of patients with blepharospasm will have difficulty opening their eyelids and they find themselves struggling to open the eyelids by raising their brows. In some of these patients, the degree of squeezing is not severe.
|
Blepharospasm: Past, Present, Future.
Anderson R.L , Patel B.C.K, Holds JB, Jordan DR.
Ophthal Plast Reconstr Surg 1998;14(5):305-317.
"I had a excellent eye lift done by Dr. Patel. He knows what he is doing and is very pleasant. Dr.Patel was easy to get an appointment and he works with you. The office staff was very pleasant and made you feel calm." D. Gull Highly recommended for eye lift surgery - Salt Lake City, UT
Information for other doctors
The early symptoms of blepharospasm include increased blink rate (77%), eyelid spasms (66%), eye irritation (55%), midfacial or lower facial spasm (59%), brow spasm (24%), and eyelid tic (22%). Symptoms commonly preceding diagnosis include tearing, eye irritation, photophobia, and vague ocular pain. While these complaints are common in the average ophthalmology practice, awareness of this disorder and proper suspicion may aid in early diagnosis. Conditions relieving blepharospasm included sleep (75%), relaxation (55%), inferior gaze (27%), artificial tears (24%), traction on eyelids (22%), talking (22%), singing (20%), and humming (19%). Comorbid diagnoses include dry eyes (49%)
and other neurologic disease (8%).
and other neurologic disease (8%).
Blepharospasm and related diseases.
Patel B.C.K., Anderson R.L.
Focal Points, Clinical Modules for Ophthalmologists 2000;18:5;1-13.
Blepharospasm: Historical Details
Henry Meige. a French neurologist described a condition in 1910 characterized by blepharospasm and facial. Mandibular, oral. lingual and laryngeal spasms and called it “spasm facial median”. Although Meige has been credited with the first description of blepharospasm. Talkow in 1870 described a patient with similar findings as did Wood in presentations at the Universitv ofPennsvlvania in the 1870s. We know from the paintings by the Flemish artist Brueghel and other clinical descriptions that the condition was known as long ago as the 16th centurv. Indeed. the frustration associated with the treatment of blepharospasm is graphicallv illustrated bv Gerold's suggestion in 1843. In a counsel of desperation, Gerold suggested treating intractable blepharospasm by "neglecting the spasm and carving a hole in the upper lid opposite the pupil through which the unfonunatc patient could peep". Whether this inauspicious procedure was ever undertaken is unknown.
How common is Blepharospasm?It is estimated that there are at least 50,000 cases of blepharospasm in the United States, with about 2000 new cases diagnosed every year. The prevalence of blepharospasm in the population is
approximately 5 in 100,000. |
Is Blepharospasm hereditory?Blepharospasm in most cases is isolated but there is a positive family history of blepharospasm in some cases. We do not think this disease is “hereditary” in that there is not a genetic transmission of this disease.
|
What is the cause of Blepharospasm?
It used to be thought that blepharospasm was a psychiatric disease. We now know that this is a neuropathologic disorder: it is caused by multiple factors which affect the central control of blinking, possibly in the basal ganglia, the midbrain and/or the brain stem. The exact site of this center is still being investigated. What makes this center become unstable in some patients is also unknown but it is known that multiple stimuli including light, corneal irritation, emotion, stress and other trigeminal stimulants exacerbate blepharospasm. The motor pathway of this complex involved the facial nucleus and the facial nerve, commonly affecting the orbicularis oculi muscle, the corrugator and the procerus muscles, with other facial muscles also being involved in many patients.
What is the normal progression of Blepharospasm?
At onset, there is increased frequency of blinking, particularly in response to a variety of common stimuli, including wind, air pollution, sunlight, noise, movements of the head or eyes, and in response to stress or the environment. Patients may complain of photophobia and ocular surface discomfort, and especially of dry eye symptoms. These symptoms progress over a variable period to include involuntary unilateral spasms, which later become bilateral. Patients may report that they are disabled to the point where they have stopped watching television, reading, driving, and/or walking. A family history positive for dystonia or blepharospasm further aids in the diagnosis. Blepharospasm commonly is associated with dystonic movements of other facial muscles. Anatomic changes associated with longstanding blepharospasm include eyelid and brow ptosis, dermatochalasis, entropion, and canthal tendon abnormalities.
How is blepharospasm managed?
|
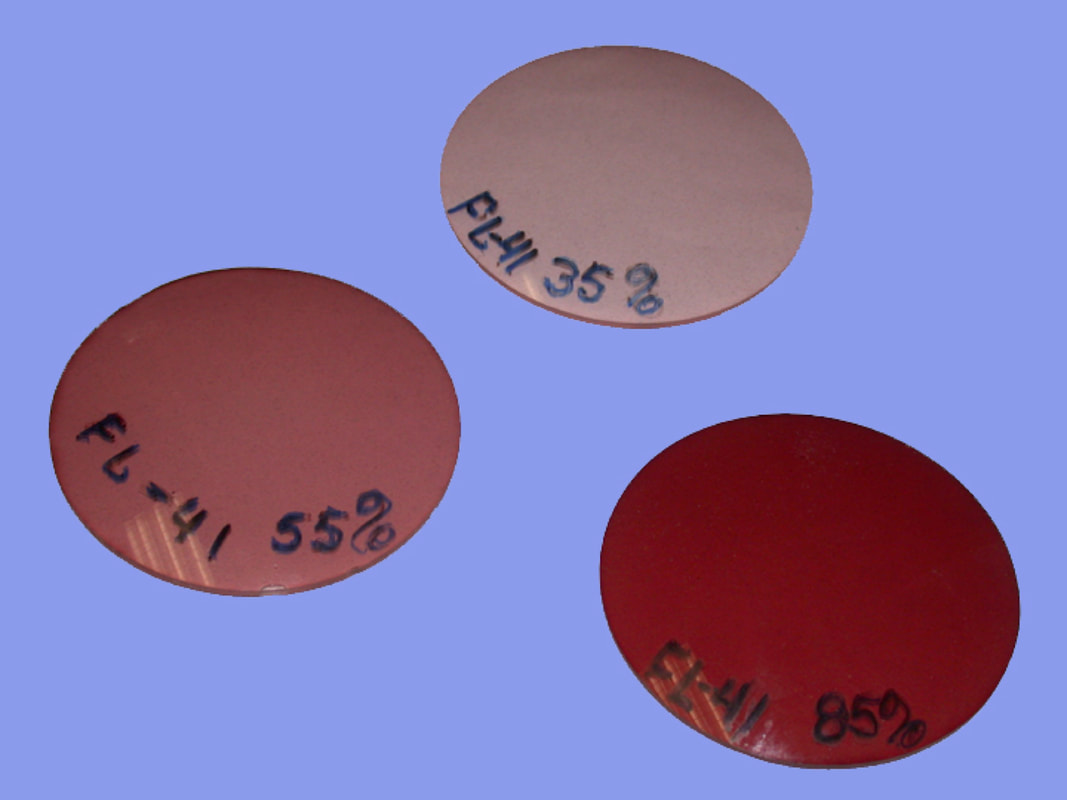
Testing different filtersDifferent FL-41 filters |
Our team at the Moran Eye Center, University of Utah showed how these FL-41 lenses are often useful in patients with light-sensitivity in blepharospasm.
Adams WH1, Digre KB, Patel BCK, Anderson RL, Warner JE, Katz BJ.The evaluation of light sensitivity in benign essential blepharospasm. Am J Ophthalmol. 2006 Jul;142(1):82-87.
Adams WH1, Digre KB, Patel BCK, Anderson RL, Warner JE, Katz BJ.The evaluation of light sensitivity in benign essential blepharospasm. Am J Ophthalmol. 2006 Jul;142(1):82-87.
What is the commonest treatment for blepharospasm?
Botulinum toxin is an approved treatment for blepharospasm and hemifacial spasm in the United States and Canada. This is a toxin produced by the bacteria Clostridium botulinum. It weakens the muscles by blocking nerve impulses transmitted from the nerve endings of the muscles. When it is used to treat blepharospasm, minute doses of botulinum toxin are injected intramuscularly into several sites above and below the eyes. The sites of the injection will vary slightly from patient to patient and according to physician preference. They are usually given on the eyelid, the brow, and the muscles under the lower lid. The injections are carried out with a very fine needle. Benefits begin in 3 - 7 days after the treatment and last for an average of three to four months. Long-term follow-up studies have shown it to be a very safe and effective treatment, with up to 90 percent of patients obtaining almost complete relief of their blepharospasm. Side effects include drooping of the eyelid (ptosis), blurred vision, and double vision (diplopia). Tearing may occur. All are transient and recover spontaneously. Providing the dose is kept small and the injections carried out at a minimum of three-month intervals, repeated treatments remain effective over a long period of time. All patients will experience an increased degree of dryness for the first few days to a few weeks after the botulinum toxin injections and will need topical artificial tears and lubricating ointment at night.
What types of botulinum toxins are available and approved?
Botulinum toxin type-A, originally called Oculinum (this same substance is now called onabotulinumtoxinA or Botox) for the treatment of strabismus and blepharospasm in 1989. The FDA also approved the use of onabotulinumtoxinA for the treatment of cervical dystonia in 2000, and for the treatment of spasticity in the flexor muscles of the elbow, wrist, and fingers in 2010.
In 2000, the FDA approved the use of a form of BoNT type-B as rimabotulinumtoxinB (or Myobloc) for the treatment of cervical dystonia. Since then, the FDA has approved two other forms of BoNT type-A. AbobotulinumtoxinA, or Dysport, was approved in 2009 for the treatment of cervical dystonia. And, in 2010, the FDA approved the use of incobotulinumtoxinA, or Xeomin, for the treatment of cervical dystonia and blepharospasm.
In 2000, the FDA approved the use of a form of BoNT type-B as rimabotulinumtoxinB (or Myobloc) for the treatment of cervical dystonia. Since then, the FDA has approved two other forms of BoNT type-A. AbobotulinumtoxinA, or Dysport, was approved in 2009 for the treatment of cervical dystonia. And, in 2010, the FDA approved the use of incobotulinumtoxinA, or Xeomin, for the treatment of cervical dystonia and blepharospasm.
Diagnosis and treatment of blepharospasm.
Patel B.C.K., Weinstein G.S., Anderson R.L.
Nesi F.A., Della Rocca R.C., Lisman R.D.. (eds)
Smith’s Ophthalmic Plastic and Reconstructive Surgery, Mosby-Year Book, Inc., Philadelphia, 2nd edition 1997;319-335.
What are the secondary effects of blepharospasm?Besides the squeezing of the eyelids (blepharospasm) and difficulty opening the eyelids (apraxia of eyelid opening), secondary effects from the squeezing as well as age-related effects can lead to brow ptosis, ptosis, dermatochalasis and lower eyelid laxity or entropion. These secondary changes may need to be addressed surgically to allow the brows and eyelids to sit at a more normal position so that the eyelids may open more effectively and also so that the effects of the botulinum toxin are acceptable.
Secondary effects of blepharospasm with ptosis, dermatochalasis, overaction of the corrugator and procerus muscles causing medial brow ptosis and lower eyelid laxity. |
When surgery is needed: Our Approach as designed by us
about 15 years ago
The traditional myectomy involved extensive incisions above the brows and an almost complete extirpation of the orbicularis oculi muscle, the corrugator muscle and the procerus muscle. Although attempts were made to re-insert the removed muscles to reduce the secondary scarring and defects created by this extractive surgery,
the results were less than ideal.
We address the problem of blepharospasm, when surgery is indicated, in a logical anatomical, physiological and individualized basis. The aim of any such surgery should be:
Our surgical approaches were developed from the cosmetic procedures we designed to perform brow lifts, eyelid cosmetic surgery, lower eyelid cosmetic surgery, cheek lifts and lower facial surgery (facelifts, etc). Using these principles and approaches, all patients are treated as if they are undergoing cosmetic surgery (to achieve as nice a cosmetic result as possible!).
The techniques involve the use of endoscopes, limited myectomy, partial manipulation of the corrugator and procerus muscles, repositioning the lower eyelids AND the cheeks and avoidance of excavations. The results look like the following photos:
the results were less than ideal.
We address the problem of blepharospasm, when surgery is indicated, in a logical anatomical, physiological and individualized basis. The aim of any such surgery should be:
- Correct the secondary effects of blepharospasm (brow ptosis, ptosis, dermatochalasis, lower eyelid laxity).
- Reduce the mass of the orbicularis that mainly contributes to the squeezing of the eyelids. This will vary from patient-to-patient and this is where careful assessment and planning are so important.
- Improve the appearance of the face.
- Protect closure of the eyelids at all cost.
- Improve lower eyelid laxity.
- Avoid defects that create hollows and excavations.
Our surgical approaches were developed from the cosmetic procedures we designed to perform brow lifts, eyelid cosmetic surgery, lower eyelid cosmetic surgery, cheek lifts and lower facial surgery (facelifts, etc). Using these principles and approaches, all patients are treated as if they are undergoing cosmetic surgery (to achieve as nice a cosmetic result as possible!).
The techniques involve the use of endoscopes, limited myectomy, partial manipulation of the corrugator and procerus muscles, repositioning the lower eyelids AND the cheeks and avoidance of excavations. The results look like the following photos:
|
Before (left) and after surgery for blepharospasm. Patient underwent endoscopic brow lifts, endoscopic weakening of the corrugator and procerus muscles, blepharoplasty with ptosis repair and limited myectomy, lower eyelid elevation and tightening, minimal lower myectomy (to prevent lower eyelid retraction and ectropion), and cheek elevation to support the lower eyelids. |
Surgical management of essential blepharospasm.
Patel BCK.
Otolaryngol Clin North Am. 2005 Oct;38(5):1075-98..
Surgical management of blepharospasm.
Patel B.C.K., Langer P., El Gazayerli E., Anderson R.L.
Naugle T.C. (ed)
Diagnosis and Management of Oculoplastic and Orbital Disorders, Kugler Publications, Amsterdam/New York; 1996:165-178.
What can I expect if I need to undergo such surgery?
All surgical procedures involve planning and preoperative and postoperative care, healing, bruising and, sometimes, additional medical or surgical aid. Overall, the outcomes to be expected in most patients are as follows:
- Reduced squeezing of the orbicularis and corrugator and procerus muscles. However, the surgery does NOT eliminate the squeezing completely.
- You will still need injections of botulinum toxin to keep the spasms under control. This is because blepharospasm is a CENTRAL disease (in the brain!) and not a peripheral disease. By performing surgery, one can only hope to reduce the effects of the central disease. This is where the earlier surgeries failed as attempts were made to completely eradicate all muscles and nerves, resulting in secondary defects and sometimes severe problems.
- EVERYONE will experience some degree of increased dryness, necessitating increased use of artificial tears and ointment and, sometimes plugging of two or more of your puncta (tear ducts).
- EVERYONE will experience some difficulty closing their eyelids to some degree. This is because of simple anatomy and physiology. If you remove some of the closing muscles (orbicularis oculi muscle), then there WILL be some weakness of closure. Furthermore, if you correct the ptosis and dermatochalasis, the lids will be more open and together with some weakness of the orbicularis muscle, there will be need to Florence Nightingale your eyes and the surrounding tissues. We will give you all the guidance. Healing is slow but sure.
- You may be more sensitive to light since your eyelids will be more open (which is a good thing!).
- If you have marked apraxia of eyelid opening, you may need frontalis slings to allow you to better open your eyelids.
Surgical Management of Essential Blepharospasm.
Patel B.C.K., Anderson R.L.
Mauriello J. (ed)
Unfavorable Results of Eyelid and Lacrimal Surgery: Prevention and Management , Butterworth Heinemann, Oxford, 2000; 181-193.
Surgical Management of Blepharospasm
Patel B.C.K.
Katowitz.J (Ed)
Facial Plastic Surgery 2005
Schedule Your Consult Today |
Frequently Asked Questions
Will the squeezing around my eyelids spread?
Over 50% of patients who develop dystonia of the eyelid closing musculature (i.e., blepharospasm) will exhibit spread to the lower face, jaw musculature, or neck within 5 years of disease onset.
Are there oral medications that can help blepharospasm?
Isolated neck lifts may be performed with sedation anesthesia or general anesthesia.
Are men and women equally affected?
The female to male ratio of involvement in this disease is 1.8:1.
When does blepharospasm present?
Two thirds of patients are 60 years or older. However, blepharospasm has also been diagnosed in children and young adults.
Will acupuncture, massage, physiotherapy or psychotherapy help?
Possibly: there are no controlled scientific studies that have shown a predictable and reliable effect of these treatments. However, if there is no active harm (there isn’t), then there is no reason for patients to try these other modalities of treatment.
I have heard I can get stem cell transplants which will cure blepharospasm?
Beware of scams.
I have heard I can get a bolt put in my head which will cure blepharospasm?
An interesting study was done by putting a surgical screw into the temple bone on the principle that many patients can keep their eyelids open by pushing at this point. Initial enthusiasm has abated as many surgeons have been unable to replicate the professed results.
I have heard that if I have complete myectomy, I won’t need botulinum toxin injections.
These claims have certainly been made. In my experience, one can improve the degree of squeezing and improve not only the ability to open the eyelids but also the effects of the botulinum toxin with a carefully considered limited myectomy. A full myectomy can lead to numerous problems of lagophthalmos, corneal exposure, conreal ulcers, ectropion, etc and is therefor only rarely undertaken. I find that very few patient can be completely weaned off botulinum toxin injections after any kind of myectomy surgery. Be careful of false promises.
What surgery would help me the most?
We designed and presented our work on a functional and aesthetic approach to surgical management of blepharospasm ONLY when specifically indicated: in this approach, a limited myectomy of the upper eyelid and the procerus and corrugator muscles is combined with an endoscopic brow lift to provide a better position and support to the brows, which makes it easier for patients to open their eyelid. It also allows future botulinum toxin injections to work better. The scars from this type of surgery are much better and results more reliable. However, a careful assessment of the response to botulinum toxins, clinical examination and assessment of the anatomical structures and health of the tear film and eyelid positions have to be considered before undertaking such surgery.
Can I become resistant to botulinum toxin?
As the disease progresses in many patients, it is often necessary to increase the dose of the botulinum toxin. True resistance is rarely seen. In some patients we may switch you from one type of botulinum toxin to another as some patients seem to get a better effect with one kind or another.
Why do I have to wait 91 days between my botulinum toxin injections?
The effects of botulinum toxin injections have been shown to take effect by day 3 to day 5 and will last for about three months. However, in some patients, the useful effects only last six weeks, and in others, up to four to five months. Taking averages into account, insurance companies have determined that they only cover injections 91 days after injections are administered.
|
Visit Patel Plastic Surgery on YouTube for more free tips!
Stay Connected With Us On Social Media
|
Find UsLocations:
Dr. BCK Patel MD, FRCS 1025E 3300S Salt Lake City, Utah 84106, USA (801) 413-3599 (phone/text) E: [email protected] bckpatel.info --------------------------------------- Dr. BCK Patel MD, FRCS 585 E Riverside Dr Suite 201 Saint George, UT 84790 (435) 215-0014 E: [email protected] Quick-Link |
Let Us answer your questions |