A comprehensive review of chalazions and chalazia with a depiction of the many different faces of chalaziaDr. BCK Patel MD, FRCS
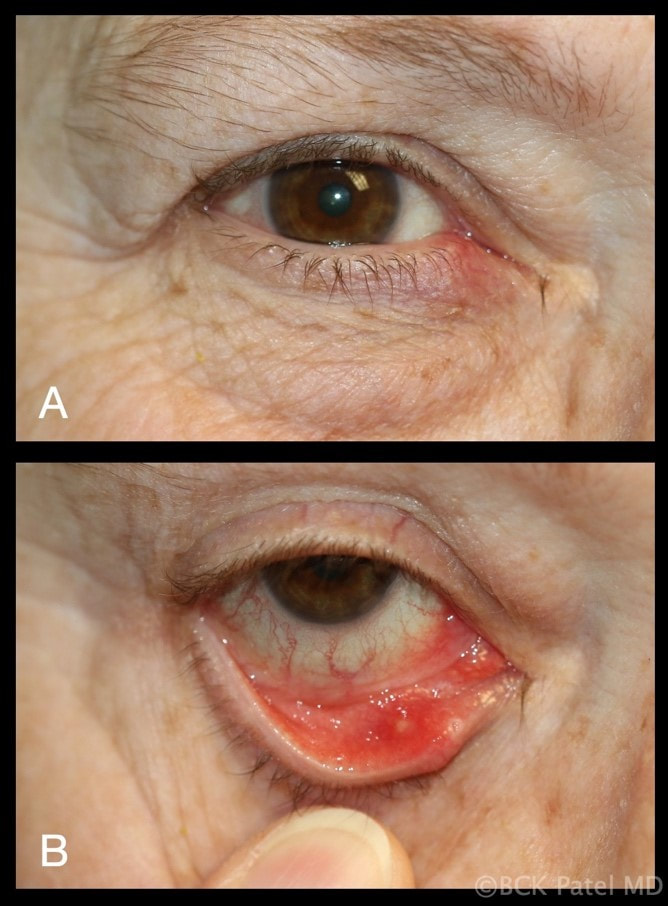
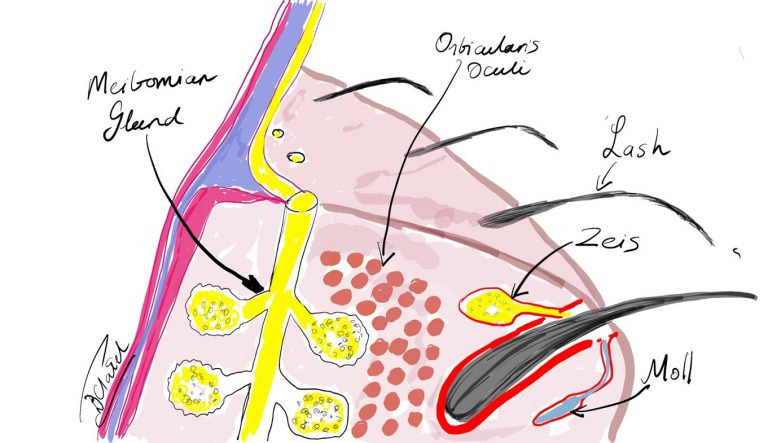
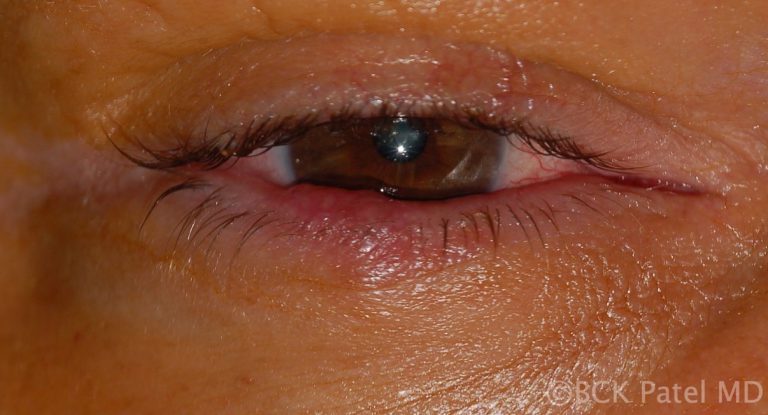
For family practice doctors, physicians, oculoplastic surgeons, ophthalmologists, residents and fellows What is a chalazion?A chalazion is initially a painless mass that develops on the eyelid. It is caused by a blockage of the Meibomian gland. The blocked gland allows the contents (lipogranulomatous material) to expand and will eventually allow the material to spread into the surrounding tissues, causing local inflammation. Initially, the chalazia are soft or rubbery but go on to become firm. Inflammation or secondary infection will lead to tenderness of the lesions. Does an initial infection of the Meibomian gland cause a chalazion to develop or is it a blocked Meibomian gland that secondarily becomes inflamed and can become infected? The exact sequence is probably both of the above in different lesions. etymology of the word "Chalazion""Khalaza" is a Greek word meaning a "small knot". The diminutive of "khalaza" is "khalazion". Therefore the singular is "chalazion" and the plural is "chalazia" or "chalazions. 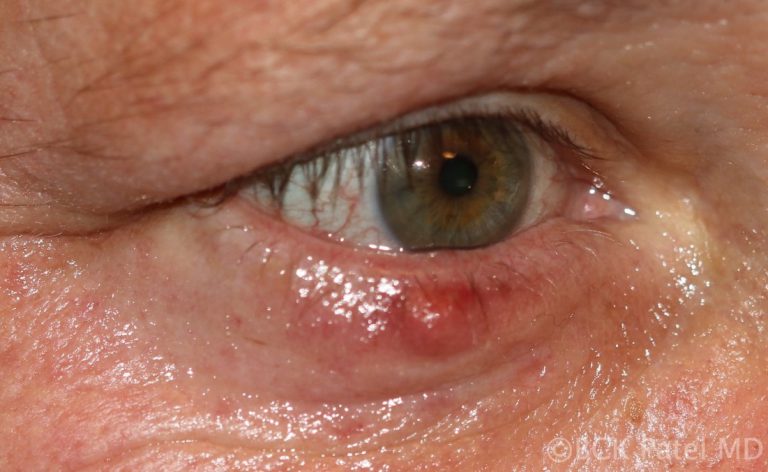 This is an acutely inflamed chalazion pointing outwards onto the skin with imminent perforation anteriorly. These are sometimes wrongly called "external hordeolum", although the word hordeolum is best reserved for a stye which is an infection of the gland of Zeis and presents anteriorly at the root of a lash SynonymsTarsal cyst Meibomian cyst External hordeolum (the word "hordeolum: is from the Latin "hordeolus" which stands for "barley" and was used because of the resemblance of the anterior chalazion to a grain of barley Internal hordeolum increased risk of developing chalazia
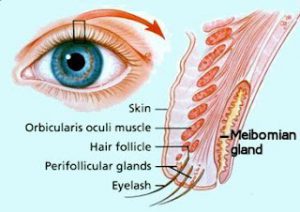
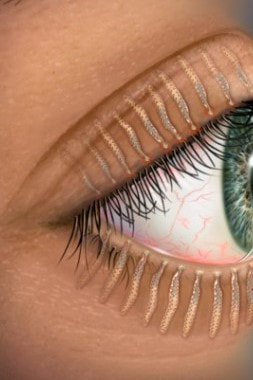
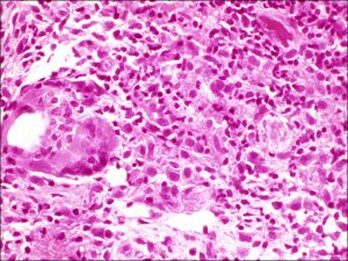
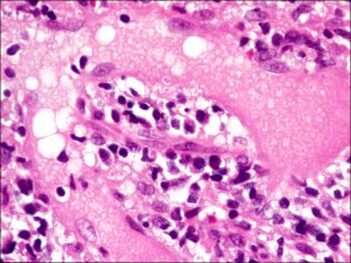
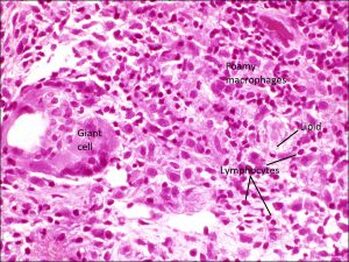
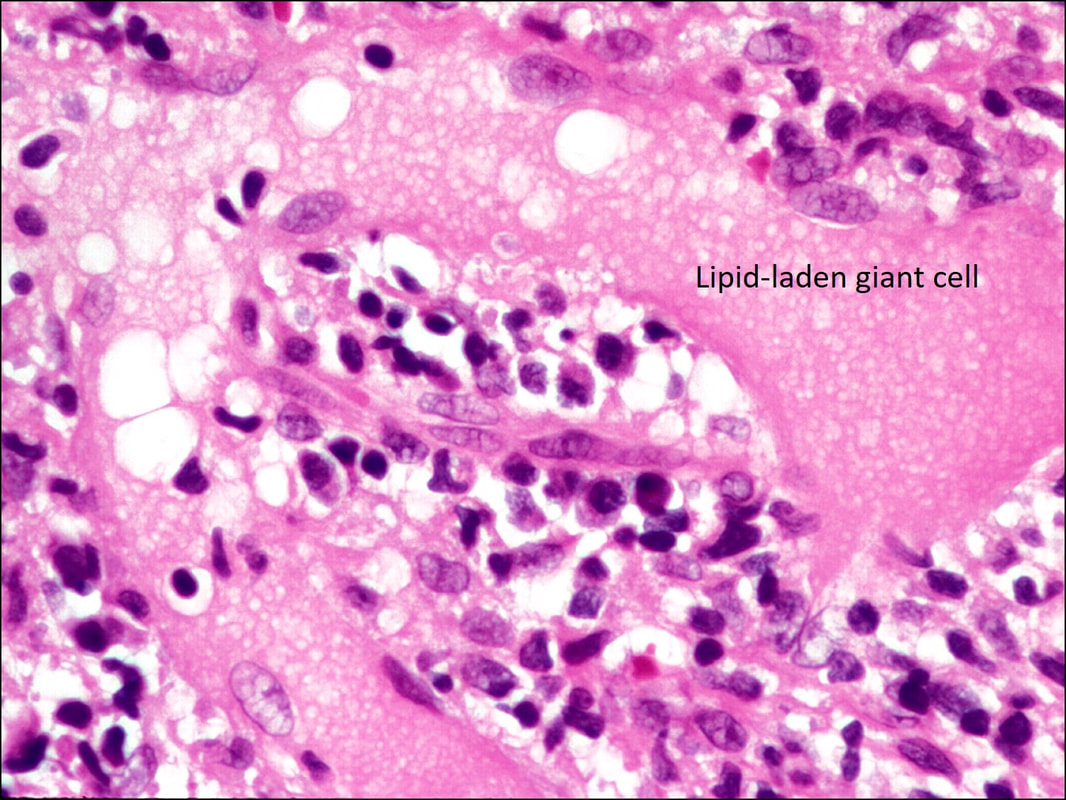
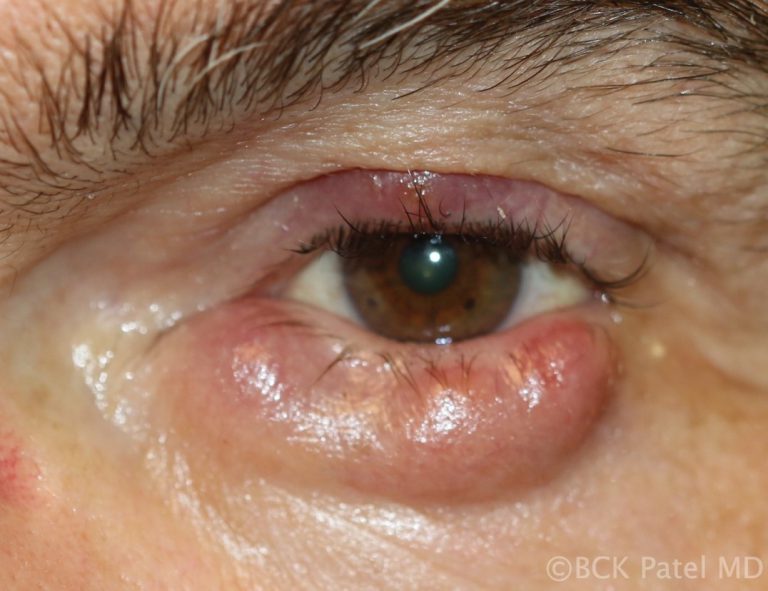
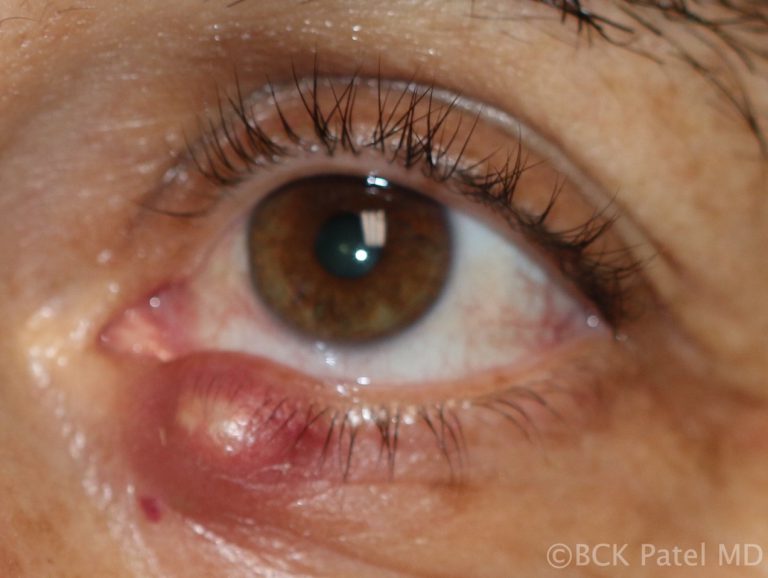
natural history of a chalazion.The initial inciting factor is blockage of a Meibomian gland. This causes the sebaceous material that is within the meibomian gland to expand. This results in a painless swelling, which is called a chalazion. Initially, the lesions are painless and expand slowly. Local tenderness occurs when there is spread of the sebaceous material to the surrounding tissues leading to local inflammation, or if there is a secondary infection which results in increased tenderness. Untreated, chalazia can increase in size and become quite firm although most will burst through to the surface (skin) or through the conjunctiva and will resolve slowly but surely. Chalazia may occur in childhood and in adults, often in the 30 - 50 age group. Predisposing factors include conditions like underlying blepharitis and acne rosacea. The use of makeup and the wearing of contact lenses does not increase the incidence of chalazia. Recently, with Covid, it has become apparent that the wearing of masks may lead to a drying effect on the eyelid margins with secondary blockage of the Meibomian glands. We have seen a significant increase in the incidence of chalazia during the Covid years 2020-2023. A large chalazion on the upper eyelid may cause a mechanical ptosis. The change in the curvature of the eyelid and also the pressure on the cornea can make it difficult to wear contact lenses. Lower eyelid chalazia can result in an ectropion with resultant epiphora (tearing). Secondary calcification may develop in the presence of chronic chalazia. Malignant transformation is extremely rare. external hordeolum A chalazion that is showing anteriorly through the skin with the appearance of a barley corn: it was therefore described as an external hordeolum. These lesions can be drained anteriorly. If they are firm, injection with steroids is reasonable. Even though they look dramatic, once they heal, the eyelid does not show any residual scarring Infections of the glands of Zeis are called styes or external hordeolum. These sebaceous oil glands open into the eyelash follicles. The term external hordeolum has erroneously been used for a chalazion that becomes infected and erodes through the skin. what are meibomian glands?Meibomian glands ae glands within the tarsus of the upper and lower eyelids. There are 30 glands in the upper eyelid and about 25 glands in the lower eyelid. They are also called tarsal glands. Meibomian glands produce an oily substance called meibum which is important in reducing the evaporation rate of tears in our tear film. These are exocrine glands: they have ducts that secrete their contents via ducts that open at the eyelid margin. They are also holocrine glands because the secretions result from lysis of the secretory glands, which causes them to release the oily substance into the Meibomian duct. Meibum not only reduces evaporation of the aqueous component of the tear film, but it also keeps the aqueous component from spilling over the edge of the eyelid by forming a film on the tear film and at the edge of the eyelid. Meibum further assists in allowing the eyelids to shut in an airtight manner. Meibomian glands: etymologyHeinrich Meibom (1638 - 1700) was a German physician who studied in France, Germany, Italy and England. He went on to become a Professor of Medicine and also a Professor of History and Poetry. He wrote Latin poetry for which he was well known. differential diagnosis of a chalazionStye Adenocarcinoma Sebaceous Gland Carcinoma Nodular basal cell carcinoma Schwannoma  This patient has a stye which is the lesion close to the eyelid margin and originates from the lash root and a chalazion which is the lower lesion. There is also a small inclusional cyst supero-medially on the upper eyelid and a seborrheic keratosis on the lateral nasal wall. There are also multiple small papillomas Histopathology of chalaziaHistopathology of the contents of a chalazion reveals a lipogranulomatous reaction with multinucleated giant cells, foamy macrophages, plasma cell, neutrophils and lymphocytes with lipid vacuoles. Histopathology will show areas of clear spaces which do not stain with H&E staining because these are lipid droplets. Older lesions may manifest fibrosis Histopathology courtesy of Prof. Nick Mamalis MD, MoranCore how do you manage chalazia presenting acutely?Patients may present with a non-tender bump on the upper or lower eyelid, in which case the lesion may cause distortion of the cornea which affects vision or may be cosmetically unacceptable. Larger lesions can cause pressure on the cornea with resultant astigmatism. Central chalazia can be in the line of sight and can also cause a mechanical ptosis interfering with the field of vision. Management:
management of chronic chalaziaAfter a few weeks, chalazia can become firm and even nodular. If left untreated, these chalazia can take weeks to months to slowly resolve. As the mass effect is often a nuisance in the presence of chronic chalazia, we usually carry out incision and drainage of the lesions with local anesthetic injection and inject the firm remnant of the chalazion with dexamethasone 4% solution. Whenever draining chalazia, the following points must be followed:
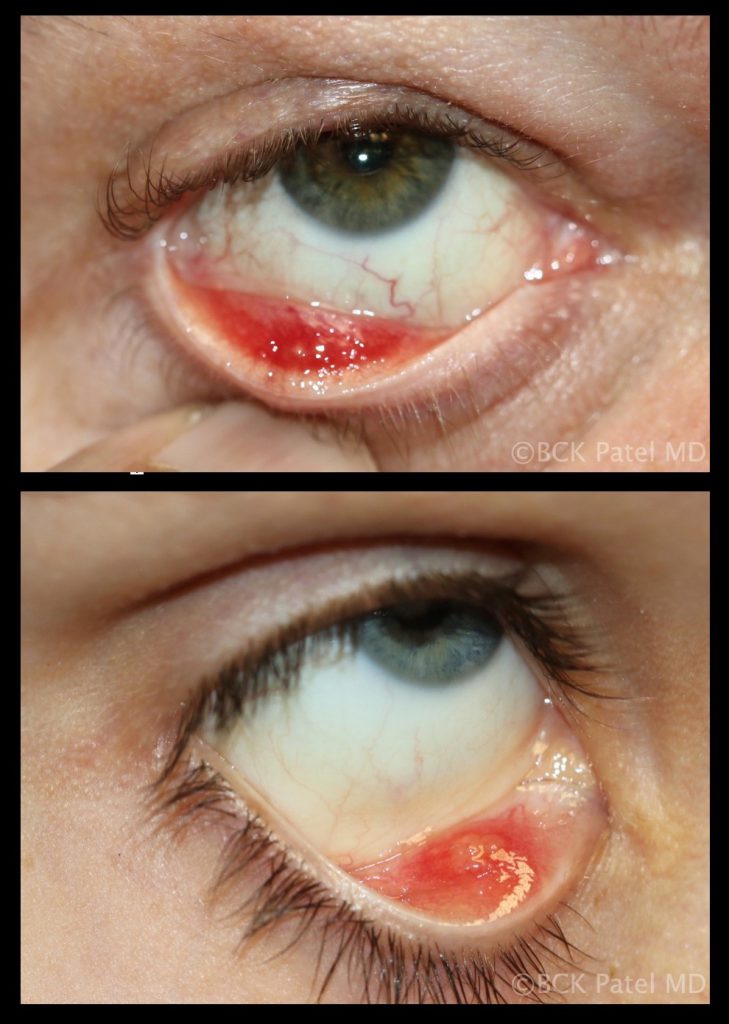
Chronic meibomianitisPatients with acne rosacea and chronic blepharitis can present with chronic meibomianitis with multiple glands being inflamed and varying number of chalazia. These patients will often present with recurring chalazia and will require topical tetracycline as well as management of the underlying condition. There may be a reduction of eyelashes even in the absence of malignancy. Treatment with intense pulsed light has been shown to improve acne rosacea and also inflammation of the eyelids. beware chronic chalazia in older patients or recurring chalaziaChronic chalazia in older patients or recurrent multiple chalazia should alert the physician to perform a biopsy as sebaceous gland carcinomas can mimic chalazia. If the chalazion has a smooth yellow surface without discomfort, it is best to biopsy the lesion. Also look for any associated loss of eyelashes. Specimens should be submitted fresh to the ophthalmic pathologist for appropriate staining looking for evidence of sebaceous gland carcinoma Chronic chalazia with pyogenic granulomas Anteriorly there appears to be no mass but eversion of the eyelid shows a posterior pyogenic granuloma. These chalazia erode through the tarsal conjunctiva causing local inflammation. Because of the granulomatous inflammation, a pyogenic granuloma may form as seen here. These need to be resected and an incision and curettage needs to be performed together with injection of steroids Chronic inflammation that bursts through the conjunctival surface can sometimes present with a pendulous inflammatory mass which is a pyogenic granuloma. These are removed surgically and the base scraped with a chalazion scoop and a steroid injection is administered chalazia with secondary cellulitisMultiple chalazia, especially in children, can spread inflammation and secondary infection into the surrounding skin resulting in a preseptal cellulitis. Indeed, whenever preseptal cellulitis is seen in children, always palpate the eyelids to exclude the presence of inflamed chalazia. Once the underlying chalazia are properly treated, the cellulitis will resolve. multiple chalaziaMultiple chalazia are seen in patients with chronic Meibomian gland disease, acne rosacea and chronic blepharitis. Multiple chalazia may also present in multiple eyelids and are thought to be hormonally related in females. When should steroids be injected into chalazia?50% of early soft chalazia will resolve just with an intralesional injection of a steroid like dexamethsone. When the lesion or lesions are firm and multiple, it is best to administer local anesthetic, perform an incision and curettage and then inject with a steroid. indications for incision and curettage
How do you perform an incision and curettage of a chalazion?Instruments
Surgical Steps:
chronic chalaziaChronic chalazia are chalazia that have been present for many weeks to months and are usually firm and painless. These are best treated with local anesthetic injection, incision and curettage, together with dexamethasone injection. We apply our two-finger firm pressure technique to break down any surrounding areas which may have chronic material in them. The patient should be warned that the bulk of the lesion will reduce in size over the subsequent few days but the final resolution can often take many weeks. Patience is key here..... giant chalazionThese are large chronic chalazia and will often look like they are occupying the whole eyelid. They will frequently emanate from multiple Meibomian glands so it is important to drain all of them properly  Giant chalazion of the left lower eyelid: these will often start as a single chalazion. With surrounding inflammation, other Meibomian glands may become involved and result in a "giant chalazion". When draining these, it is important to identify and drain all the surrounding glands that may be involved Chalazia in children Multiple chalazia in eyelids. Children will often get multiple chalazia in the same eyelid and multiple eyelid. No cause has been identified. When chronic, incision and curettage is reasonable. We evert all four eyelids to ensure all the Meibomian glands have been squeezed as there will frequently be low-grade insipissation in some glands. It is important to explain to the parents that other glands can become blocked days or weeks after any drainage has been performed. Recent studies show that Azithromycin may be beneficial for some cases Children will often present with chalazia, often multiple and frequently recurrent. There is no known cause of this and most will settle with conservative management discussed above. Parents can get frustrated by the recurrent chalazia that some children get. We always reassure them that they eventually resolve and do not leave any underlying scarring of the eyelids. In some cases oral antibiotics like Azithromycin are indicated  Children will often be brought in with small "bumps" on the eyelid where the family will complain that the chalazia "have not gone away". Chronic chalazia can take weeks to month to resolve. Topical steroids may be needed but mostly it is a case of allowing the body to continue its healing process. Haraka haraka haina baraka chalazion in patients with skin of colorWhereas the management of chalazia in patients who have skin of color is the same as in white Caucasians, care must be taken not to inject with steroids superficially as hypopigmentation may occur. references
1 Comment
|
AuthorDr. BCK Patel MD, FRCS |
- Home
- Locations
-
Conditions
- Aging Of The Face
- Aging of Lower Eyelids
- Aging of the Forehead and Brows
- Aging of Upper Eyelids
- Aging of the Cheeks
- Aging of the Neck
- Aging of the Lips
- Aging of the Mouth
- Aging of the Chin
- Aging of Eyelashes
- Aging of the Hands
- Aging Of Skin Colour
- Aging Of Hair
- Aging of the Jowls
- Aging of Men
- Aging of the Skin
- Aging of Veins and Vessels
- Scars
-
Cosmetic
- Facelift
- Browlifts
- Lower Blepharoplasty
- Upper Blepharoplasty
- Midface Lift/Hammock Lift
- Necklift
- Cosmetic Surgery for Men
- Lip Lines
- Lips
- Mouth
- Neck Liposuction
- Fat Transfer
- Skin Resurfacing
- Cheeks
- Removal of Moles, Lesions, Tags, Cysts and Blemishes
- Facial Implants
- Otoplasty, Ear Pinning, or Bat-Ear Repair
- Complications?
-
Reconstruction
- Acquired Ptosis and Dermatochalasis
- Congenital Ptosis
- Ptosis in Myasthenia Gravis
- Blepharophimosis Syndrome
- Entropion
- Ectropion
- Thyroid Eye Disease
- Nasolacrimal Duct Obstruction
- Skin Tumors
- Orbital Tumors
- Blepharospasm
- Pterygium
- Anophthalmos and Microphthalmos
- Enucleation and Evisceration
- Exenteration
- Symblepharon
- Congenital Anomalies - Lid Disorders
- Acne Rosacea
- Trauma
- Infections
-
Non Invasive
- Photorejuvenation
- Aerolase Laser
- Botox
- Radiesse
- Restylane
- Juvederm
- Fractional Carbon Dioxide CO2 Laser
- Fractional Resurfacing Lasers: Erbium lasers
- Laser Hair Removal
- Kybella
- Chemical Peels
- XEOMIN ®
- Voluma
- LATISSE EYELASH TREATMENT
- Leg Veins and Spider Vein Treatment
- Sculptra
- Neck and Chest Cosmetic Concerns
- Dysport
- Accent Radiofrequency
- Microdermabrasion and Light Chemical Peels
- Melasma
- Laser Tattoo Removal
- Color and Texture Issues – Brown Spots on Face, Redness
- Scars and Acne
- Permanent Cosmetic Makeup
- Resources
- About
- Blog
- Contact
VIDEOS
links
www.hammocklift.com
WWW.PATELFACELIFT.COM
www.englishsurgeon.com
www.drbhupendrapatel.com
bckpatel.info
WEBOFSCIENCE
researchgate
GOOGLE SCHOLAR
linktr.ee
Patel Plastic Surgery . Copyright 2024 . All Rights Reserved