|
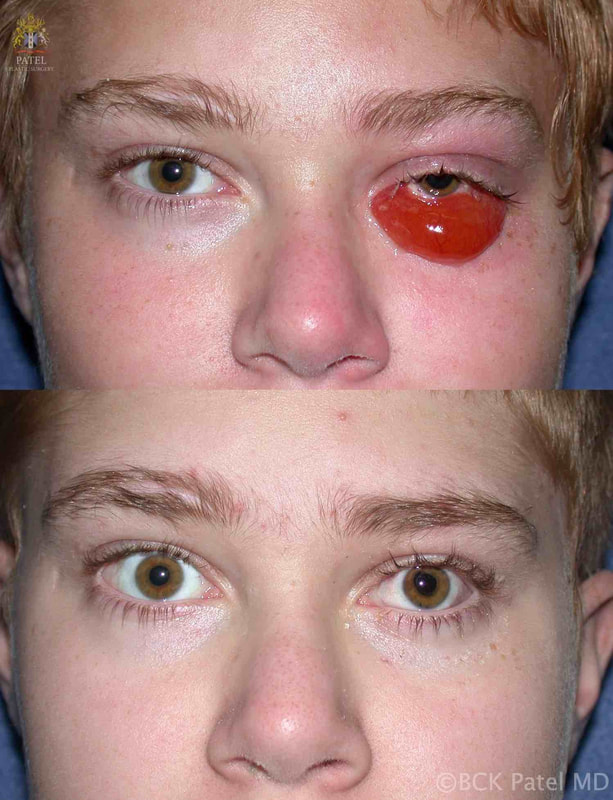
BCK Patel MD, FRCS For Residents, Fellows, Plastic Surgeons, Oculoplastic Surgeons What is chemosis?Conjunctival chemosis is the collection of fluid under the conjunctiva, resulting in a blister-like swelling of the conjunctiva. what conditions can cause or predispose to chemosis?Chemosis is seen after periocular and periorbital surgery such as lower eyelid blepharoplasty, cheek lift, Hammock lift, lateral canthoplasty, entropion repair, ectropion repair and, indeed, whenever there is manipulation of the tissues of the lower eyelids and/or cheeks. Chemosis may occur after transcutaneous or transconjunctival blepharoplasty Chemosis may be seen with orbital inflammation as seen in thyroid orbitopathy, myositis and idiopathic orbital inflammation Chemosis may be seen with an intraorbital tumor Chemosis is often seen after midfacial and orbital trauma Chemosis occurs in the presence of allergy Chemosis is seen in the presence of infection of the conjunctiva, eyelid or orbit what is the cause of chemosis?Inflammation due to trauma, infection of underlying disease is thought to increase the risk of chemosis. Furthermore, anything (like surgery or trauma) that interferes with the flow of the lymphatics from the eyelids and the orbit can result in chemosis. Chemosis is more common when the lateral canthus is operated upon and is also more common in patients who already have laxity of the conjunctiva (conjunctivochalasis) which is associated with sun damage and age. Poor eyelid closure predisposes to conjunctival exposure with secondary conjunctivochalasis and these patients are more likely to develop chemosis after any periorbital surgery. pathogenesis of chemosis after blepharoplastyTrauma to the eyelid (blepharoplasty) and the lymphatics and also any disruption of the conjunctiva can lead to local inflammation and delay in the outflow of fluid via the lymphatics. The resultant chemosis causes the conjunctiva to become prominent, dry and have more inflammation with further separation of the conjunctiva from the underlying tissues (Tenon's fascia and slcera). The elevation of the conjunctiva is limited by the limbus. Interference with tear flow and tear film results in further dehydration of the exposed conjunctiva. Dryness of the adjoining cornea at the limbus because of adjoining conjunctival swelling and interference with normal eyelid closure can lead to corneal thinning and the formation of a Dellen (thinned cornea). This further inflames the tisues with worsening of the chemosis. grading of chemosisChemosis is best graded as mild, moderate and severe. Mild Chemosis: there is mild conjunctival elevation with underlying fluid. The conjunctiva does not ride over the eyelid margin and does not interfere with eyelid closure.  Mild chemosis where the conjunctiva is just elevated from the underlying attachments but does not go over the eyelid margin and does not interfere with eyelid closure. This is often seen after many eyelid and cosmetic facial procedures where there is dissection around the orbicularis oculi muscles and the eyelid retractors Moderate Chemosis: the protruding conjunctiva now rides to and just over the eyelid margin and more prominently over the sclera. The eyelid closure is still adequate Severe Chemosis: in severe chemosis, there is marked elevation of the conjunctiva together with the conjunctival lining now interfering with the excursion of the upper eyelid and with separation of the lower eyelid from the globe with an in adequate eyelid closure Management of chemosisManagement of predisposing factors that can lead to chemosis: Underlying conditions that should be considered and managed prior to surgery or during surgery:
Anti-inflammatory medication prior to surgery and during surgery may include topical steroid drops and/or ointment, oral steroids, intravenous steroids. Peroperative Management of Chemosis Towards the end of a facial cosmetic or reconstructive plastic surgical procedure, especially when the surgery involves the eyelids and/or orbit, the conjunctiva should be examined as it is not uncommon to detect early chemosis at this stage. Mild Chemosis: if mild chemosis is noted at the end of the procedure, the following two approaches may be taken: 1. Imbrication of the conjunctiva to the inferior fornix and underlying Tenon's fascia: here interrupted simple 6-0 catgut sutures may be used to close the space between the conjunctiva and the Tenon's capsule or inferiorly at the inferior fornix. The closure of the subconjunctival space using interrupted sutures will help reduce postoperative chemosis. 2. A partial temporary tarsorrhaphy: this may be performed using one or more sutures to hold the upper and lower eyelids together, especially over the area where the chemosis is forming. 3. A one-snip or several-snip procedure: this is performed with both of the above techniques to reduce the conjunctival chemosis. The incision is made through the conjunctiva and the fluid is milked out using moist Q-tips. One or more incisions may be made and the Tenon's fascia may need to be perforated to adequately drain the collected fluid. 4. For extensive chemosis: it is reasonable to raise the conjunctiva and the Tenon's capsule at the limbus and dissect these tissues off the sclera and milk the liquied out of the extensive chemotic tissues. Interrupted simple 7-0 vicryl sutures can be use to reapproximate the conjunctiva at the limbus or tissue glue may be used. Most of the fluid will be under the conjunctiva but in severe cases, there will also be fluid below the Tenon's capsule At the end of these procedures, it is reasonable to put the patient on topical steroid drops (tobradex drops, maxitrol drops or Pred Forté 1% drops and topical steroid ointment for a week. management of postoperative chemosis Mild Chemosis: In the presence of mild chemosis, there is usually a lateral collection of fluid under the conjunctiva, without interference of eyelid closure and without any Dellen formation. If the eyelid closure is complete with minimal discomfort, simple topical steroid drops and steroid ointment are prescribed and we commence our patients on the "upward pressure" regime three times a day for two minutes at a time and review the clinical appearance two weeks later. Topical lubrication with preservative-free drops and ointment at night is always added after eyelid surgery for the first three to four weeks in all patients. Moderate Chemosis: Moderate chemosis with show elevation of the conjunctiva to and just at the edge of the lower eyelids with some underlying dryness of the cornea and interference with the tear film. In these patients, a vasoconstrictive topical drop is applied (phenylephrine2.5%), topical steroid drops and ointment are commenced, and the patient is asked to increase the topical preservative-free lubricants during the daytime and ontment (refresh-pm ointment) at night. Mechanical closure of the eyelids allows the conjunctiva to be kept moist, the cornea is protected and inflammation reduced. This is done with two eye patches which are applied once the eyelids are properly closed. The patches may be left on for 24 hours and repeated as needed. We routinely put our patients on a Medrol dose pack if extensive periorbital surgery is being performed. This includes patients undergoing Facelifts, Hammock Lifts, upper and lower blepharoplasty or lower blepharoplasty with cheek lifts. Severe Chemosis Severe chemosis can vary from the level where it interferes with eyelid closure to marked prolapse of the edematous conjunctiva over the edge of the eyelid with exposure of the conjunctiva on attempted closure of the eyelids. In these cases, it is imperative to treat the patient using the following steps: 1. Topical local anesthetic is administered (proparacaine drops, anesthetic gel) together with phenylephrine hydrochloride ophthalmic solution 2.5% which aids in vasoconstriction 2. Injection of 1% lidocaine with epinephrine may be used if the patient is particularly sensitive. Approximately 0.3 - 0.5 cc are injected into the area of the chemosis 3. A one-snip incision is performed using westcott sutures and holding the conjunctiva and the Tenon's capsule with a fine toothed (0.3 mm ) forceps 4. There will be egress of fluid: this can be encouraged using two Q-tips which can be rolled from the inferior fornix upwards and lateral-to-medial and medial-to-lateral 5. We will usually put the patient on a Medrol dose pack at this point If adequate reduction in the chemosis is achieved, we often suture the eyelids together with a simple 6-0 catgut suture over the area of the maximal swelling. These appose the upper and lower eyelids and the sutures will "dissolve" in a few days. The closure of the eyelids partially or completely will enhance the resolution of the chemosis. With mild, moderate or severe chemosis, we will usually institute our "upward pressure on the lower eyelids" treatment as illustrated in the video below. The art of patching an eyePatching an eye is often necessary after eyelid surgery or when treating chemosis. It is important to learn to patch an eye properly so that the eyelids are adequately closed with no risk of the patch rubbing against the cornea. Steps in applying a Proper Patch:
Chronic chemosis after cosmetic surgerySome patients will develop chronic chemosis which may persist or even worsen several weeks after surgery. The eye will look relatively white and there will be minimal or no inflammation. The circle of swelling-secondary dryness of the cornea-formation of dellen will continue and it is important to release the fluid more aggressively. In these cases, it is reasonable to incize the conjunctiva at the limbus and undermine the conjunctiva and the Tenon's fascia and "milk" the fluid out with Q-tips. In the presence of chronic chemosis, the amount of fluid that can be drained will be more limited and patience will be required when performing the "milking" of the fluid. All these patients will require a suture tarsorrhaphy to keep the eyelids adequately closed, the cornea protected and to allow the dellen to recover. Ointment is applied three times a day at the medial opening between the eyelids. mechanical and paralytic causes of chronic chemosisMechanical Causes: if there is an inability of the eyelids to close because of muscle weakness, eyelid laxity or tissue distortion, this needs to be corrected to allow proper closure of the eyelids and also to allow the muscle action of the eyelids to allow egress of the fluid. If the lateral canthus is disassociated from the lateral orbital rim. the upper and lower eyelids will not be able to correctly move and close: the appearance has been described as "fishmouthing" when the patient is observed blinking. The lateral canthus needs to be reattached to the lateral orbital rim to create the proper position of the eyelids and correct "tension" of the orbicularis oculi muscle. Paralytic Causes: surgical dissection involved in the performance of blepharoplasty or midface surgery can cause temporary or permanent and partial or more severe facial nerve injury. The orbicularis muscle tone will be reduced, and with it the blink. In such patients, a partial blink can lead to exposure, inflammation and secondary chemosis, especially if there has already been underlying conjunctivochalasis. In many such patients, as the branches of the buccal and zygomatic facial nerve recover, so does the closure of the eyelids and the chemosis. Mecanical disruption of lymphatic flow: in transconjunctival and even transcutaneous dissection, lympatic flow may be affected with resultant slow egress of fluid from under the conjunctiva. The exact lymphatic flow from the subconjunctival space is not yet adequately understood. Severe chemosis related to traumaWhen there is extensive facial, orbital and soft tissue trauma, severe chemosis can occur. It is multifactorial:
1 Comment
Clarisse
7/22/2024 09:10:49 pm
Hi, is severe chemosis related to trauma can be cured? How?
Reply
Leave a Reply. |
AuthorDr. BCK Patel MD, FRCS |
- Home
- Locations
-
Conditions
- Aging Of The Face
- Aging of Lower Eyelids
- Aging of the Forehead and Brows
- Aging of Upper Eyelids
- Aging of the Cheeks
- Aging of the Neck
- Aging of the Lips
- Aging of the Mouth
- Aging of the Chin
- Aging of Eyelashes
- Aging of the Hands
- Aging Of Skin Colour
- Aging Of Hair
- Aging of the Jowls
- Aging of Men
- Aging of the Skin
- Aging of Veins and Vessels
- Scars
-
Cosmetic
- Facelift
- Browlifts
- Lower Blepharoplasty
- Upper Blepharoplasty
- Midface Lift/Hammock Lift
- Necklift
- Cosmetic Surgery for Men
- Lip Lines
- Lips
- Mouth
- Neck Liposuction
- Fat Transfer
- Skin Resurfacing
- Cheeks
- Removal of Moles, Lesions, Tags, Cysts and Blemishes
- Facial Implants
- Otoplasty, Ear Pinning, or Bat-Ear Repair
- Complications?
-
Reconstruction
- Acquired Ptosis and Dermatochalasis
- Congenital Ptosis
- Ptosis in Myasthenia Gravis
- Blepharophimosis Syndrome
- Entropion
- Ectropion
- Thyroid Eye Disease
- Nasolacrimal Duct Obstruction
- Skin Tumors
- Orbital Tumors
- Blepharospasm
- Pterygium
- Anophthalmos and Microphthalmos
- Enucleation and Evisceration
- Exenteration
- Symblepharon
- Congenital Anomalies - Lid Disorders
- Acne Rosacea
- Trauma
- Infections
-
Non Invasive
- Photorejuvenation
- Aerolase Laser
- Botox
- Radiesse
- Restylane
- Juvederm
- Fractional Carbon Dioxide CO2 Laser
- Fractional Resurfacing Lasers: Erbium lasers
- Laser Hair Removal
- Kybella
- Chemical Peels
- XEOMIN ®
- Voluma
- LATISSE EYELASH TREATMENT
- Leg Veins and Spider Vein Treatment
- Sculptra
- Neck and Chest Cosmetic Concerns
- Dysport
- Accent Radiofrequency
- Microdermabrasion and Light Chemical Peels
- Melasma
- Laser Tattoo Removal
- Color and Texture Issues – Brown Spots on Face, Redness
- Scars and Acne
- Permanent Cosmetic Makeup
- Resources
- About
- Blog
- Contact
VIDEOS
links
www.hammocklift.com
WWW.PATELFACELIFT.COM
www.englishsurgeon.com
www.drbhupendrapatel.com
bckpatel.info
WEBOFSCIENCE
researchgate
GOOGLE SCHOLAR
linktr.ee
Patel Plastic Surgery . Copyright 2024 . All Rights Reserved